Breast and Cervical Cancer Prevention and Early Detection Program
FREE PAP SCREENING
AND MAMMOGRAPHY!
AND MAMMOGRAPHY!
- Mammograms
- Clinical breast exam Pap test
- Test for detection of Human Papillomavirus (HPV)
- Diagnostic mammography
- Sonomamography (ultrasound)
- Consultation with a surgeon
- Breast biopsies
- Routine Pap test (screening) and Pap test (diagnosis)
- Colposcopy
- Biopsies
- Treatment of precancerous lesions of the cervix
- Be between the ages of 21 and 64
- Not qualify for the Puerto Rico health plan
- Not have a private health plan
- Meet the income requirements
- Women 65 years of age or older who do not have Medicare or Medicare Part B
If you want to know if you qualify for the program or receive more information, you can call 787-522-3265

About Us
The PR Breast and Cervical Cancer Prevention and Early Detection Program is sponsored by the Centers for Disease Control and Prevention (CDC). The program provides free screening tests such as mammograms and Pap smears, as well as diagnostic procedures for breast and cervical cancer, to eligible women. We also offer patient navigation and case management services, and educational activities for the community and health professionals. The program has physicians and imaging centers across the island by region. The program’s headquarters are located in the trust building in San Juan.
Breast Cancer
What is the breast?
The inside of the breast is made up of ducts, lobes, lobules, fatty tissue, and lymph nodes. There are approximately 15 to 20 groups of lobes. These are in turn made up of smaller sections called lobules that are responsible for milk production. Ducts are thin tubes that carry milk from the lobule to the nipple. Between the lobules and the ducts is a space made up of fat and fibrous tissue.
Retrieved from:
www.google.com.pr/images/breast
What is breast cancer?
Breast cancer is an abnormal growth of cells that originates in the breast tissue. There are two common types of breast cancer:
- Ductal cancer (ductal carcinoma): This is the most common and begins in the ducts that carry milk from the breast to the nipple.
- Lobular cancer: This begins in the milk-producing lobules of the breast.
Breast cancer statistics in Puerto Rico
The Puerto Rico Central Cancer Registry reported the following data on breast cancer:
It is the most common type of cancer in women, with approximately 2,455 women dying from this condition between 2014 and 2018, and by 2022.
It is the most common cause of cancer death in women, with 403 women dying from this condition that same year.
Risk factors
No woman is immune from breast cancer. The cause of breast cancer is unknown, but there are some risk factors that may increase the chance of developing breast cancer.
These factors include:
Risk factors that cannot be modified or changed:
- Being a woman
- Aging
- Inheriting certain genetic changes (alterations in the genes associated with breast cancer, the BRCA1 and BRCA2 genes)
- Family history of breast cancer from the mother or father in the first generation (mother, sister, or daughter)
- Having had breast cancer before
- Dense breast
- Benign (noncancerous) breast problems
- First menstruation before age 12
- Menopause after age 55
- History of radiation to the chest
- Exposure to the drug diethylstilbestrol (DES) to prevent miscarriage
Risk factors that can be modified or changed:
- Having children late in life (after age 30) or not having had children
- Use of hormone therapy for birth control or menopause
- Obesity
- Not exercising regularly or physical inactivity
- Consumption of alcoholic beverages
How is breast cancer detected?
Tests to detect breast cancer include:
Early detection test:
Mammography: is an X-ray of the breast that allows the detection of lumps (masses) that are not palpable, when there are no symptoms yet and the probability of a cure is greater. Mammography is the RECOMMENDED method for the early detection of breast cancer.
Other screening tests:
Clinical exam: This is when the doctor or nurse looks at and feels the breasts to detect the possible presence of a lump or other changes. This exam is NOT recommended for the early detection of breast cancer, it is optional.
Breast self-knowledge (better known as the Breast Self-Exam): This is when you look at and feel your breasts to detect possible lumps and changes in the size or shape of the breast. This exam is NOT recommended for the early detection of breast cancer, it is optional.
Guidelines for early detection of breast cancer recommend the following tests and procedures:
When is the best time to have a mammogram?
When undergoing a mammogram, please keep the following instructions in mind:
- Bring your health insurance information with you on the day of the exam.
- Do not schedule your mammogram the week before your menstrual period, as your breasts may be more tender then.
- It is recommended that you do not wear deodorant, powder, perfume, or lotion on your underarms or breasts on the day of your mammogram, as this may cause staining on your x-ray.
- Tell your doctor or the technologist performing the exam about any symptoms or problems you may have with your breasts.
- If possible, bring your previous mammograms with you in case your radiologist needs them to evaluate your exam.
- Before the exam, you will be asked to remove jewelry and clothing from the waist up, and you will be provided with a front-opening gown to cover up.
- On the day of your exam, preferably wear a comfortable two-piece outfit (skirt and blouse or pants and blouse).
- If you are taking any medication, use it unless otherwise instructed.
- Always inform your doctor or radiology technician if there is a possibility you are pregnant.
Related Links
National Cancer Institute
Breast Cancer Basics
American Cancer Society
Educational Material:
Breast Cancer: What You Should Know
It’s your life. No one better than you to take care of it.
Instituto Nacional del Cáncer: https://www.cancer.gov/espanol
Centro para la prevención y control de enfermedades (CDC por sus siglas en inglés) https://www.cdc.gov/spanish/index.html
Other screening tests
Cervical Cancer
What is cervical cancer?
Cervical cancer is an abnormal growth of cells in the cervix (neck of the uterus). Almost all cases of cervical cancer are caused by infection with some type of human papillomavirus (HPV). This type of cancer is preventable because there is a vaccine against the human papillomaviruses (HPV) related to this cancer. In addition, there are tests that can detect changes in the cells of the cervix before they become cancer.
Cervical cancer statistics in Puerto Rico
The Puerto Rico Central Cancer Registry reported the following data on cervical cancer:
- It is the seventh most common type of cancer in women; in 2022, 196 women were diagnosed with this condition.
- In the same year, 46 women died from this condition.
Risk factors
The main risk factor for cervical cancer is infection with certain types of human papillomavirus (HPV). This virus is transmitted primarily through sexual contact. In the United States, an estimated 13 million new cases of HPV occur each year, and there are currently more than 42 million people infected.
- HPV is the most common sexually transmitted infection.
Eight out of 10 people will be infected with HPV at some point in their lives. - HPV affects men and women equally.
- HPV is most common in adolescents and young adults between the ages of 15 and 24.
- There are more than 130 types of HPV. Of these, approximately 40 types can infect the genital and anal areas of men and women, as well as the mouth and throat.
- In most cases, HPV causes no symptoms, so people do not know they have the virus.
- Some HPV types cause genital warts (low risk), and others cause precancerous changes or cancer (high risk).
- HPV can cause cancer of the cervix, vulva, vagina, anus, penis, and oropharynx.
In addition to HPV, other factors increase the risk of developing this type of cancer. These factors include:
- Starting sexual activity at an early age
- Having had many sexual partners
- Not having regular Pap smears
- Cigarette smoking
- History of multiple births
- Diet low in fruits and vegetables
- Weak immune system
- Use of oral contraceptives (the pill)
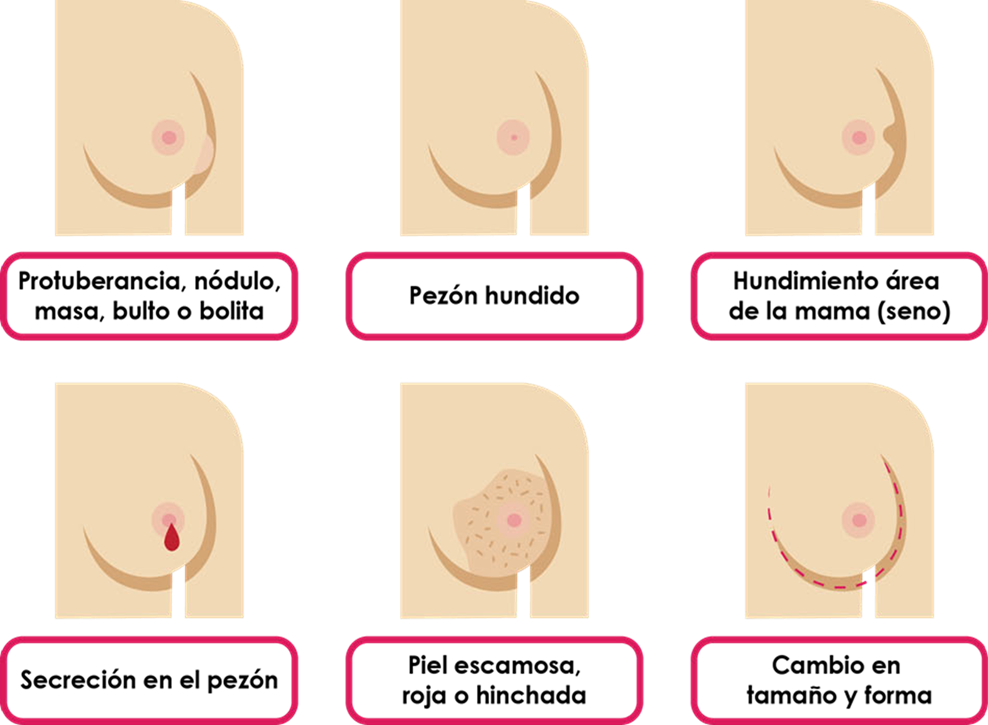
Signs or symptoms
In the early stages, cervical cancer usually does not present signs or symptoms. However, in advanced stages, we may find the following symptoms:
- Vaginal bleeding after sexual intercourse
- Vaginal bleeding that is not related to menstruation
- Vaginal bleeding after menopause
- Vaginal bleeding after pelvic exam
- Pelvic pain
- Pain during sexual intercourse
How is cervical cancer detected?
Cervical cancer screening tests are recommended for all women ages 21 to 65. These tests are very simple and can be performed by your doctor in his or her office or clinic. The doctor uses a plastic or metal instrument to widen the vagina so he or she can examine the cervix and take a sample of cells. These cells are sent to a lab to be examined to determine if they are abnormal.
Guidelines for early detection of cervical cancer recommend the following tests or procedures:
When is the best time to get tested for early detection?
When undergoing a mammogram, please keep the following instructions in mind:
- . Bring your health insurance information with you on the day of the exam.
- Do not schedule your mammogram the week before your menstrual period, as your breasts may be more tender then.
- It is recommended that you do not wear deodorant, powder, perfume, or lotion on your underarms or breasts on the day of your mammogram, as this may cause staining on your x-ray.
- Tell your doctor or the technologist performing the exam about any symptoms or problems you may have with your breasts.
- If possible, bring your previous mammograms with you in case your radiologist needs them to evaluate your exam.
- Before the exam, you will be asked to remove jewelry and clothing from the waist up, and you will be provided with a front-opening gown to cover up.
- On the day of your exam, preferably wear a comfortable two-piece outfit (skirt and blouse or pants and blouse).
- If you are taking any medication, use it unless otherwise instructed.
- Always inform your doctor or radiology technician if there is a possibility you are pregnant.
How can I prevent cervical cancer?
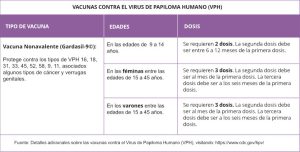
Vaccination against Human Papillomavirus (HPV)
Human Papillomavirus (HPV) is the main cause of cervical, vaginal, vulvar and anal cancer. Infection with certain types of HPV and cervical cancer can be prevented by vaccination against this virus. These are broken down below:
There is a vaccine to prevent HPV types related to cancer and genital warts:
- Nonavalent Vaccine (Gardasil-9©):
- Protects against HPV types 16, 18, 31,33,45,52,58,9,11.
- It is recommended for women aged 9-45 years for the prevention of HPV infection, precancerous and cancerous lesions of the vulva, vagina and anus, cervix or cervix.
- It is recommended for men aged 9-45 years for the prevention of HPV infection, precancerous and cancerous anal lesions.
- Both males and females between the ages of 9 and 14 years require two doses, the second dose should be administered between 6 to 12 months after the first dose.
- Both men and women between the ages of 15 and 45 years require three doses, 0.1 and 6 months apart.
- The vaccine is most effective if given before the onset of sexual activity when the likelihood of exposure to HPV is lower, which is why current guidelines recommend that the vaccine be given between 11 and 12 years of age.
- The vaccine is safe.
- The HPV vaccine “DOES NOT CURE, IT PROTECT”.
- Talk to your doctor about this vaccine.
For more information visit the following websites:
Educational Resources for the
Community
Educational Resources for Providers